Protecting Senior Vision: 5 Common Eye Diseases
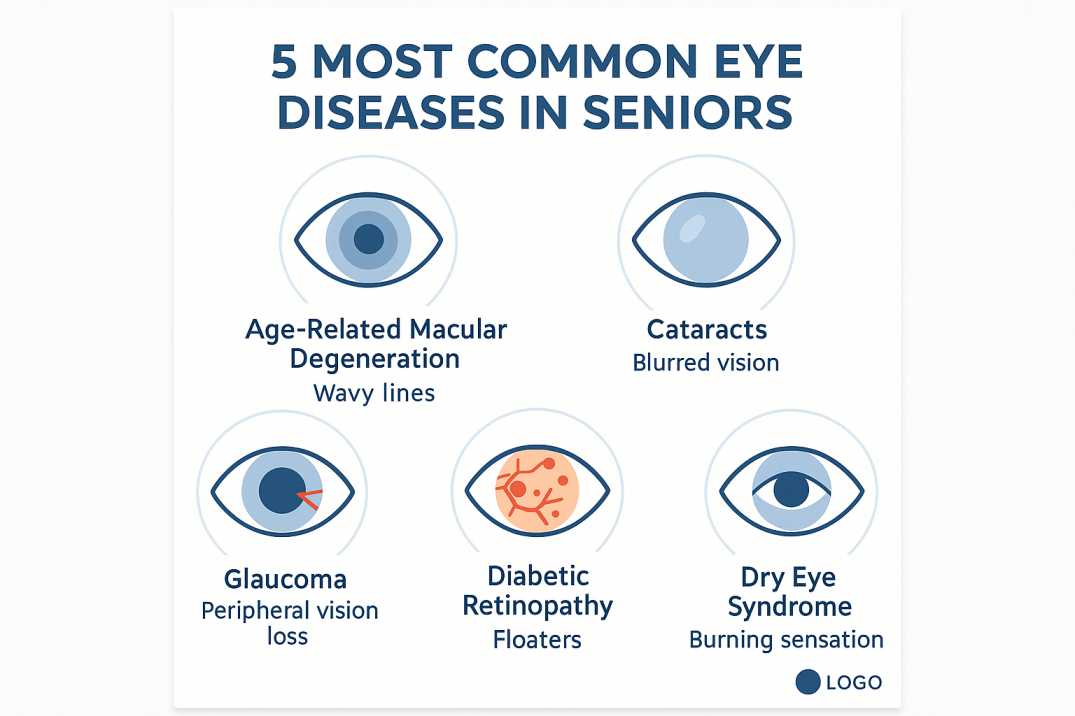
Bottom Line: Age-related macular degeneration, cataracts, glaucoma, diabetic retinopathy, and dry eye syndrome are the five most common eye diseases affecting seniors over 60. Most develop silently without early symptoms, making annual comprehensive eye exams essential for early detection and preventing vision loss.
Understanding Your Risk: What Every Senior Should Know
As we age, our eyes become more vulnerable to serious conditions that can affect independence and quality of life. Nearly one in three adults over 65 experiences some form of vision-impairing eye disease.
The five most common eye diseases affecting seniors—age-related macular degeneration, cataracts, glaucoma, diabetic retinopathy, and dry eye syndrome—often develop silently, showing no warning signs until significant damage has occurred.
The good news? Early detection through regular eye exams can significantly protect your vision and prevent complications. This comprehensive guide will help you recognize warning signs, understand your risks, and take action to preserve your vision for years to come.
Understanding Age-Related Eye Health Changes
Your eyes change naturally as you age, but knowing the difference between normal aging and serious disease is crucial for maintaining your vision and independence.
Normal Aging vs. Disease
Many people experience routine vision changes after age 40, including needing more light to read, difficulty with close-up work, and increased glare sensitivity. These common adjustments don’t always signal disease. However, certain symptoms warrant immediate attention from an eye care professional.
When to Schedule an Eye Exam:
- Sudden changes in vision quality
- Straight lines appearing wavy or distorted
- New floaters or flashes of light
- Progressive vision loss
- Difficulty distinguishing colors
- Significantly impaired night vision
The American Optometric Association recommends annual comprehensive eye examinations for everyone over age 60, even without symptoms. Why? Many eye diseases develop silently in their early stages when treatment is most effective.
1. Age-Related Macular Degeneration (AMD): The Leading Cause of Vision Loss
What Is AMD?
Age-related macular degeneration is the leading cause of vision loss in people over 50 in the Western world. This condition damages the macula—the central part of your retina responsible for sharp, detailed vision needed for reading, driving, and recognizing faces.
Types of AMD
Dry AMD (Geographic Atrophy)
The dry form accounts for 70-90% of AMD cases and progresses more slowly than wet AMD. It develops in three stages:
- Early Stage: Tiny yellow deposits (drusen) form under the retina with no symptoms
- Intermediate Stage: Larger drusen appear; some people notice mild vision changes
- Late Stage: Significant central vision loss occurs
Wet AMD (Neovascular AMD)
Wet AMD involves abnormal blood vessels growing under the macula, leading to blood and fluid leakage that causes rapid central vision loss. Though less common, it’s more severe and progresses faster.
Early Warning Signs of AMD
Watch for these specific symptoms:
- Straight lines appearing wavy (a key warning sign requiring immediate attention)
- Blurred or fuzzy areas in your central vision
- Dark or empty spots in the center of your visual field
- Difficulty seeing in low lighting
- Colors appear less vibrant than before
- Trouble recognizing faces at normal distances
Risk Factors You Can Control
While age increases AMD risk, several modifiable factors play important roles:
- Smoking: Doubles your risk of developing AMD
- High blood pressure: Damages blood vessels in the eye
- Poor diet: Lack of leafy greens and omega-3 fatty acids
- Obesity: Increases progression to advanced stages
- Sun exposure: UV damage accumulates over time
Recent Research and Treatment Advances
The landmark AREDS and AREDS2 studies have shown that specific vitamin formulations can reduce the risk of progression to advanced AMD by about 25 percent in people with intermediate or advanced disease. The AREDS2 formula includes:
- Vitamin C: 500 mg
- Vitamin E: 400 IU
- Lutein: 10 mg
- Zeaxanthin: 2 mg
- Zinc (as zinc oxide): 80 mg
- Copper (as cupric oxide): 2 mg
Critical Notes: These supplements are only beneficial for people with intermediate or advanced AMD—they don’t prevent early AMD or stop early AMD from progressing. The AREDS2 formula replaced beta-carotene from the original AREDS formula because beta-carotene increases lung cancer risk in current and former smokers. Always consult your eye care provider before starting any supplement regimen, as these high-dose vitamins may interact with medications or cause side effects in some individuals.
2. Cataracts: Clouding the Lens of Life
Understanding Cataract Development
Cataracts are cloudy areas in the normally clear lens of your eye. Think of your eye’s lens like a camera lens—when it becomes clouded, images appear blurry or faded. More than 24 million Americans age 40 and older currently have cataracts, and this number is expected to reach 50 million over the next three decades. By age 80, more than half of Americans will have cataracts or have had cataract surgery.
How Cataracts Form
As you age, proteins in your lens break down and clump together, creating cloudy patches. This natural process happens gradually, often over years. Most people don’t notice vision changes until the cloudiness affects a larger portion of the lens.
Recognizing Cataract Symptoms Early
Early detection helps you plan treatment when it’s most convenient for your lifestyle.
Early Signs:
- Needing brighter light for reading or close work
- Increased sensitivity to glare from headlights or sunlight
- Halos appearing around lights at night
- Colors appear faded or yellowed
- Frequent changes in eyeglass prescription
Progressive Symptoms:
- Cloudy, blurred, or dim vision
- Double vision in one eye
- Difficulty driving at night
- Trouble distinguishing between similar colors (like navy and black)
Types of Cataracts
Nuclear Cataracts: Form in the center of the lens; most common with aging
Cortical Cataracts: Develop in the lens cortex with spoke-like clouding
Posterior Subcapsular Cataracts: Form at the back of the lens; progress faster and affect reading vision more quickly
Modern Cataract Treatment
The only effective treatment for cataracts is surgical lens replacement, which has become one of the safest and most successful procedures in medicine. During surgery, your clouded natural lens is removed and replaced with a clear artificial lens called an intraocular lens (IOL).
What to Expect:
- The outpatient procedure takes about 15 minutes per eye
- Little to no discomfort during recovery
- Vision improvement is often noticed within days
- Advanced IOL options can correct distance and near vision
3. Glaucoma: The “Silent Thief of Sight”
Why Glaucoma Is So Dangerous
Glaucoma is called the “sneak thief of sight” because people usually don’t notice vision loss until the disease is very advanced. This group of eye diseases damages your optic nerve—the vital connection between your eye and brain.
How Glaucoma Develops
Most glaucoma occurs when fluid pressure inside the eye slowly rises, though recent findings show glaucoma can also occur with normal eye pressure. Either way, the result is the same: progressive, irreversible damage to the optic nerve fibers.
Types of Glaucoma
Open-Angle Glaucoma (Most Common)
Develops slowly over the years as the eye’s drainage system becomes less efficient. You typically won’t notice symptoms until significant peripheral vision loss has occurred.
Angle-Closure Glaucoma (Acute)
A sudden blockage causes rapid pressure buildup. This is a medical emergency requiring immediate treatment to prevent permanent vision loss.
Silent Disease, Serious Consequences
The challenge with glaucoma is that it often develops painlessly with no obvious symptoms until there’s a significant loss of peripheral vision. By the time you notice vision changes, substantial irreversible damage has already occurred.
Late-Stage Symptoms Include:
- Gradual loss of peripheral (side) vision
- Tunnel vision in advanced stages
- Halos around lights (more noticeable in dim lighting)
- Difficulty adjusting to different lighting conditions
- Eye pain or headaches (primarily with angle-closure glaucoma)
Who’s at Higher Risk?
Several factors increase your glaucoma risk:
- Age over 60: Risk increases significantly
- Family history: Having a relative with glaucoma raises your risk
- African American heritage: Higher prevalence and earlier onset
- High eye pressure: Detected during routine eye exams
- Thin corneas: Measurable during comprehensive exams
- Diabetes and high blood pressure affect blood flow to the optic nerve
Treatment Options
While damage from glaucoma can’t be reversed, progression can be slowed or stopped with:
- Prescription eye drops: Reduce eye pressure daily
- Laser treatments: Improve fluid drainage
- Surgical procedures: Create new drainage pathways
The key is early detection through regular dilated eye exams, which allow your eye doctor to examine your optic nerve and measure eye pressure before symptoms develop.
4. Diabetic Retinopathy: When Diabetes Affects Your Eyes
The Diabetes-Eye Connection
Diabetic retinopathy is the leading cause of blindness in American adults of working age. If you have diabetes—whether Type 1 or Type 2—high blood sugar levels can damage the tiny blood vessels in your retina over time.
Understanding the Progressive Stages
Diabetic retinopathy progresses through four stages, from mild nonproliferative retinopathy with tiny areas of swelling to severe proliferative retinopathy with new abnormal blood vessel growth.
Early Stages:
- Microaneurysms (tiny bulges in blood vessels)
- Small areas of vessel blockage
- Usually no symptoms
- Detectable only through a dilated eye exam
Advanced Stages:
- Abnormal new blood vessels grow
- These vessels are fragile and leak easily
- Blood leaks into the vitreous (gel inside the eye)
- Scar tissue can form, pulling on the retina
- Risk of retinal detachment increases
Warning Signs and Symptoms
The challenging aspect of diabetic retinopathy is that it develops slowly, often with no early warning signs. Many people have significant retinal damage before noticing vision changes.
Symptoms of Advanced Diabetic Retinopathy:
- Floaters (dark spots or strings floating in vision)
- Blurred or fluctuating vision
- Dark or empty areas in your vision
- Difficulty seeing colors clearly
- Progressive vision loss
Prevention Through Blood Sugar Management
The risks of diabetic retinopathy can be reduced through the management of blood sugar, blood pressure, and cholesterol. Maintaining target ranges significantly decreases your risk of developing retinopathy or slows its progression.
Protective Strategies:
- Keep A1C levels within your target range
- Monitor and control blood pressure
- Maintain healthy cholesterol levels
- Get annual dilated eye exams (more frequently if retinopathy is detected)
- Exercise regularly and maintain a healthy weight
- Don’t smoke
Treatment Advances
Modern treatments can prevent vision loss when diabetic retinopathy is caught early:
- Anti-VEGF injections: Block abnormal blood vessel growth
- Laser photocoagulation: Seals leaking vessels and prevents new growth
- Vitrectomy: Removes blood from the vitreous in advanced cases
5. Dry Eye Syndrome: More Than Just Irritation
Why Dry Eye Becomes More Common with Age
Dry eye occurs when the tear glands don’t work well, causing a stinging or burning sensation as if something is in the eye. This condition is common as people get older, especially for women experiencing hormonal changes.
Understanding Your Tear System
Your eyes need a consistent, healthy tear film to:
- Keep the eye surface smooth and clear
- Wash away debris and microorganisms
- Provide nutrients to the cornea
- Reduce infection risk
When this system breaks down, discomfort and vision problems follow.
Recognizing Dry Eye Symptoms
Dry eye can significantly impact your daily activities and quality of life.
Common Symptoms:
- Persistent dry, scratchy, or gritty sensation
- Burning or stinging in the eyes
- Excessive tearing (the eye’s response to irritation)
- Stringy mucus in or around the eyes
- Eye fatigue and difficulty reading
- Blurred vision that improves with blinking
- Discomfort when wearing contact lenses
Contributing Factors
Understanding what worsens dry eye helps you take preventive action:
- Aging: Natural decrease in tear production
- Medications: Antihistamines, decongestants, blood pressure medications
- Environmental conditions: Wind, smoke, dry air, air conditioning
- Screen time: Reduces blink rate, allowing tears to evaporate
- Medical conditions: Sjögren’s syndrome, rheumatoid arthritis, thyroid disorders
- Previous eye surgery: Including LASIK
Effective Management Strategies
Most people find relief through a combination of approaches.
At-Home Care:
- Use a humidifier to add moisture to indoor air
- Take regular breaks during computer work (20-20-20 rule)
- Protect eyes from wind with wraparound sunglasses
- Stay hydrated by drinking plenty of water
- Include omega-3 fatty acids in your diet
Professional Treatments:
- Artificial tears: Over-the-counter drops provide relief
- Prescription eye drops: Reduce inflammation and increase tear production
- Punctal plugs: Tiny devices block tear drainage to keep eyes moist longer
- Intense pulsed light therapy: Treats meibomian gland dysfunction
- LipiFlow treatment: Unclogs blocked oil glands in eyelids
The Power of Early Detection: Your Action Plan
Why Regular Eye Exams Are Non-Negotiable
Many people don’t notice any signs or symptoms in the early stages of eye diseases. A dilated eye exam performed by an eye care professional is the only way to find some common eye diseases while they’re easier to treat—and before they cause vision loss. The American Optometric Association recommends annual comprehensive eye examinations for everyone over age 60.
Recommended Screening Schedule
Ages 40-54: Every 2-4 years (more often with risk factors)
Ages 55-64: Every 1-3 years
Age 60 and older: Annually (as recommended by the American Optometric Association)
With diabetes or high blood pressure: At least annually, regardless of age
What Happens During a Comprehensive Eye Exam
A thorough examination includes multiple tests beyond just checking your vision.
Visual Acuity Test: Measures how clearly you see at various distances
Dilated Eye Exam: Eye drops widen pupils so your doctor can examine the retina and optic nerve for damage or disease
Tonometry: Measures eye pressure to screen for glaucoma
Visual Field Test: Checks peripheral vision
Optical Coherence Tomography (OCT): Creates detailed images of retinal layers
Fundus Photography: Documents the appearance of your retina for comparison over time
Protecting Your Vision: Prevention Strategies That Work
Lifestyle Modifications for Healthy Eyes
Research consistently shows that certain lifestyle choices significantly reduce your risk of eye disease.
Nutrition for Eye Health
Studies show that high levels of antioxidants and zinc can reduce some people’s risk of developing advanced AMD by about 25 percent. Focus on:
- Leafy greens: Kale, spinach, collards (rich in lutein and zeaxanthin)
- Colorful vegetables: Carrots, sweet potatoes, bell peppers
- Fish: Salmon, tuna, mackerel (omega-3 fatty acids)
- Citrus fruits: Oranges, grapefruit (vitamin C)
- Nuts and seeds: Almonds, sunflower seeds (vitamin E)
Physical Activity
Regular exercise improves blood flow to the eyes and helps control conditions like diabetes and high blood pressure that can damage vision. Aim for 150 minutes of moderate activity weekly.
Smoking Cessation
Tobacco use can increase your risk of eye problems like cataracts and AMD. Quitting at any age reduces your risk, and the benefits begin almost immediately.
Sun Protection
UV radiation contributes to cataract formation and may increase AMD risk. Protect your eyes by:
- Wearing wraparound sunglasses that block 99-100% of UVA and UVB rays
- Adding a wide-brimmed hat for extra protection
- Never looking directly at the sun
Managing Chronic Conditions
Diseases like diabetes and high blood pressure can cause eye problems if not controlled or treated. Work with your healthcare providers to keep these conditions well-managed.
Technology and Your Eyes: The Digital Age Challenge
The 20-20-20 Rule for Screen Time
If you spend a lot of time at the computer or focus on one thing, take a break every 20 minutes to look about 20 feet away for 20 seconds to prevent eye strain.
Reducing Digital Eye Strain
With increased screen time, many people experience:
- Eye fatigue and discomfort
- Blurred vision
- Headaches
- Dry, irritated eyes
Protective Strategies:
- Position screens 20-26 inches from your eyes
- Adjust screen brightness to match ambient lighting
- Use larger fonts and increase contrast
- Consider blue light filtering glasses or screen protectors
- Blink frequently and completely
Resources and Scientific Citations
This article is based on rigorous scientific research and authoritative medical sources. Below are three key resources that informed our comprehensive guide:
1. Age-Related Eye Disease Studies (AREDS/AREDS2) – National Eye Institute
Source: National Institutes of Health, National Eye Institute
Link: https://www.nei.nih.gov/research/clinical-trials/age-related-eye-disease-studies-aredsareds2
The landmark AREDS and AREDS2 clinical trials, conducted by the National Eye Institute from 1992 to present, established that specific nutritional supplements can reduce the risk of AMD progression by approximately 25 percent. These studies involved thousands of participants and provided the evidence-based foundation for current AMD prevention recommendations. The research demonstrated that a formulation containing vitamin C, vitamin E, lutein, zeaxanthin, zinc, and copper significantly benefits people with intermediate or advanced macular degeneration.
2. Common Eye Diseases in Aging Adults – Centers for Disease Control and Prevention
Source: CDC Vision and Eye Health
Link: https://www.cdc.gov/vision-health/about-eye-disorders/index.html
The CDC’s comprehensive overview of common eye disorders provides critical prevalence data and public health information about age-related eye diseases. This resource confirms that cataracts, AMD, diabetic retinopathy, and glaucoma are the leading causes of blindness and visual impairment in the United States, with risk dramatically increasing after age 65. The CDC emphasizes that early detection through regular dilated eye exams is essential for preventing vision loss.
3. Senior Vision Guidelines – American Optometric Association
Source: American Optometric Association
Link: https://www.aoa.org/healthy-eyes/eye-health-for-life/senior-vision
The AOA’s evidence-based clinical practice guidelines provide the foundation for recommended eye exam frequency and comprehensive care standards for seniors. Their research confirms that annual eye examinations for everyone over age 60 are critical because many serious eye diseases develop painlessly with no symptoms in their early, most treatable stages. The AOA represents more than 50,000 doctors of optometry and sets the professional standards for quality eye care in the United States.
Additional Medical Review: This article’s medical information has been reviewed for accuracy against current clinical guidelines and peer-reviewed research as of 2025. All statistics, dosage recommendations, and clinical advice reflect the most recent evidence-based standards from leading ophthalmological and optometric organizations.
When to Seek Immediate Medical Attention
While some eye symptoms develop gradually, others require urgent care. Contact an eye care professional immediately if you experience:
- Sudden vision loss or significant vision changes
- Sudden onset of many floaters or flashes of light
- A curtain or a shadow moving across your field of vision
- Severe eye pain
- Sudden red eye with blurred vision
- Eye injury
- Double vision
- Sudden sensitivity to light
These symptoms could indicate serious conditions like retinal detachment, acute angle-closure glaucoma, or other conditions requiring immediate intervention to prevent permanent vision loss.
Taking Control of Your Eye Health: Your Next Steps
Protecting your vision doesn’t have to be overwhelming. Start with these simple, actionable steps:
1. Schedule Your Comprehensive Eye Exam Today
If you haven’t had a dilated eye exam in the past year and you’re over 60, make that appointment today. Early detection is your best defense against vision loss. Schedule your exam online or call Poudre Valley Eyecare.
2. Know Your Family History
Many eye diseases have hereditary components. Understanding your family’s eye health history helps your doctor assess your risk and tailor screening recommendations. Make a list of any relatives who’ve had:
- Macular degeneration
- Glaucoma
- Cataracts (at a young age)
- Diabetic retinopathy
- Other eye conditions
3. Document Your Baseline
Keep records of your eye exam results, including:
- Vision measurements and prescription
- Eye pressure readings
- Photos of your retina
- Recommended follow-up schedule
- Any diagnosed conditions
This documentation helps track changes over time and facilitates care if you see multiple providers.
4. Make One Lifestyle Change This Week
You don’t need to overhaul your entire life at once. Start with one or two modifications:
- This week: Add leafy greens (spinach, kale) to your daily diet
- This month: Invest in quality UV-blocking sunglasses and wear them daily
- This quarter: Schedule an annual physical to monitor blood pressure and blood sugar
- This year: If you smoke, set a quit date and talk to your doctor about cessation resources
5. Create Your Eye Health Action Plan
Next 7 Days:
- Schedule a comprehensive eye exam (if overdue)
- Purchase UV-protective sunglasses
- Add eye-healthy foods to your grocery list
- Review current medications with the doctor
Next 30 Days:
- Complete scheduled eye exam
- Implement the 20-20-20 rule for screen time
- Start AREDS2 supplements (if recommended by your doctor)
- Share this article with family members
Next 3 Months:
- Follow up on any findings from the eye exam
- Establish regular eye-healthy habits
- Schedule next annual exam
- Monitor for any vision changes
6. Stay Informed But Not Overwhelmed
Understanding eye diseases helps you recognize warning signs, but remember that your eye care professional is your partner in maintaining vision health. Don’t hesitate to call with questions or concerns between appointments.
The Bottom Line: Your Vision Is Worth Protecting
As you age, you may notice changes that affect your eyes and vision, but regular exams can protect your eye health. The five most common eye diseases affecting seniors—age-related macular degeneration, cataracts, glaucoma, diabetic retinopathy, and dry eye syndrome—share one critical characteristic: they’re most treatable when caught early.
You have more control over your eye health than you might think. Through regular comprehensive exams, healthy lifestyle choices, and prompt attention to warning signs, you can significantly reduce your risk of vision loss and maintain your independence for years to come.
Remember: Most serious eye diseases develop silently. Don’t wait for symptoms—schedule that comprehensive eye exam and take the first step toward protecting one of your most precious senses.
Poudre Valley Eyecare has served the Fort Collins community for over 25 years, providing comprehensive eye care for all ages. We accept Medicare and Medicaid and welcome new patients. Schedule your comprehensive eye examination today to protect your vision for tomorrow.
FAQs
-
-
Cataracts, glaucoma, age-related macular degeneration (AMD), diabetic retinopathy, and presbyopia are the most common eye diseases in seniors.
-
Please note: None of the above should be considered medical advice. If you’re having any concerns about your vision, please reach out to us immediately or see your primary care provider.