Flashes and Floaters: When Are They a Warning Sign?
Introduction
Have you ever noticed specks drifting across your vision when looking at a bright sky or white wall? Or perhaps you’ve experienced sudden flashes of light that seem to come from nowhere? These visual phenomena, known as flashes and floaters, affect up to 76% of people at some point in their lives, making them one of the most common eye-related concerns patients bring to our Fort Collins practice.
While most flashes and floaters represent harmless signs of normal eye aging, they can sometimes signal serious conditions requiring immediate medical attention. Understanding the critical difference between routine symptoms and emergency warning signs could literally save your vision.
At Poudre Valley Eyecare, we’ve been Fort Collins’ trusted partner in comprehensive eye health for over 25 years. Our Medicare and Medicaid-accepting practice has evaluated thousands of patients with flashes and floaters, giving us unique insight into when these symptoms require urgent intervention versus routine monitoring.
In this evidence-based guide, you’ll learn:
- How to distinguish normal flashes and floaters from emergency symptoms
- Risk factors that increase your likelihood of serious complications
- When to seek same-day versus routine eye care
- Latest treatment advances for bothersome symptoms
- Practical strategies for managing benign floaters
Understanding Eye Floaters
What Are Eye Floaters?
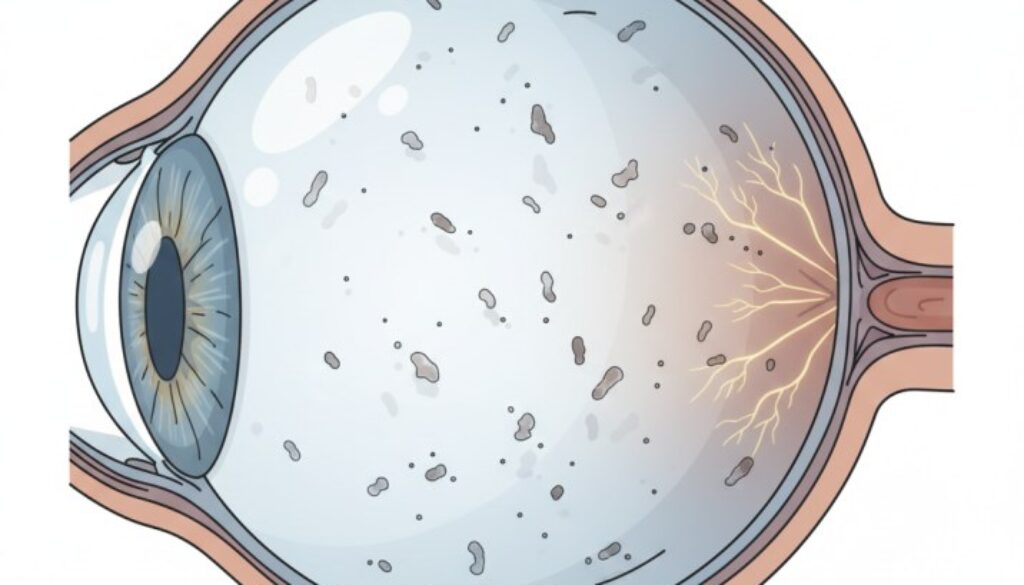
Eye floaters appear as small, dark shapes that drift across your field of vision, particularly noticeable against bright backgrounds. These moving shadows take various forms:
- Dots and spots: Small, round dark specks
- Thread-like strands: Thin, squiggly lines resembling hair
- Cobweb patterns: Web-like shapes that move with eye movement
- Ring shapes: Circular or oval outlines (often called Weiss rings)
- Cloud-like formations: Irregular, translucent patches
Important note: While floaters appear to float in front of your eyes, they actually exist inside your eye, casting shadows on your retina—the light-sensitive tissue that captures visual images.
The Science Behind Floaters
Your eye contains a clear, gel-like substance called vitreous humor that fills approximately 80% of your eye’s volume. This gel maintains your eye’s spherical shape and provides an optical pathway for light to reach your retina.
The vitreous consists primarily of water (98%) with a network of collagen fibers that provide structural integrity. As we age—typically beginning around age 50—this gel undergoes natural changes:
- Liquefaction: The gel gradually becomes more liquid
- Syneresis: Collagen fibers separate from the surrounding matrix
- Aggregation: These separated fibers clump together
- Shadow formation: The clumped fibers cast shadows on your retina, creating the visual perception of floaters
This process, known as vitreous degeneration, occurs in nearly everyone as part of normal aging. However, the timing and extent can vary based on individual factors like myopia, eye trauma, and genetic predisposition.
Understanding Eye Flashes
What Are Eye Flashes?
Eye flashes manifest as brief bursts of light that appear suddenly in your peripheral vision. Patients commonly describe them as:
- Lightning streaks: Jagged lines of light at the edge of vision
- Camera flashes: Sudden, bright bursts resembling photography flashes
- Sparkles or stars: Brief, twinkling points of light
- Arc-shaped lights: Curved bands of illumination
- Flickering sensations: Rapid on-off light perception
Unlike floaters that persist and drift, flashes typically appear suddenly and disappear within seconds, most commonly occurring in dim lighting conditions or with eye movement.
The Mechanism Behind Flashes
Flashes occur when something other than light stimulates your retina mechanically. The most common cause involves the vitreous gel pulling on retinal tissue during the natural aging process.
Here’s what happens:
- Vitreous shrinkage: As the gel contracts with age, it begins to separate from the retina
- Mechanical stimulation: Areas where the vitreous remains attached create traction on the retinal tissue
- Neural response: Since the retina lacks pain receptors, this mechanical stimulation triggers light-sensing cells
- Flash perception: Your brain interprets these signals as flashes of light
Think of it like pressing on your closed eyelids and seeing “stars”—physical pressure on the retina creates the sensation of light even in complete darkness.
Normal vs. Emergency Symptoms
Understanding when flashes and floaters represent normal aging versus potential emergencies is crucial for protecting your vision. Knowing these distinctions can mean the difference between preserving your sight and facing permanent vision loss.
When Flashes and Floaters Are Usually Harmless
Normal floater characteristics:
- Develop gradually over months or years
- Remain stable in number and size
- Move predictably with eye movement
- Don’t interfere with daily activities
- Become less noticeable over time through brain adaptation
Typical harmless flashes:
- Occur occasionally with sudden head movements
- Last only seconds
- Happen infrequently without accompanying symptoms
- May be related to migraine auras (lasting 10-20 minutes)
Reassuring patterns:
- Long-standing symptoms without change
- Bilateral (both eyes) gradual development
- No associated vision loss or visual field defects
- Symptoms that improve with rest
Critical Emergency Warning Signs
Contact an eye care professional immediately if you experience:
Sudden onset symptoms:
- A shower of new floaters appears within hours
- Dramatic increase in floater size or density
- Large, dense floaters that obstruct central vision
Vision-threatening changes:
- Dark curtain or shadow moving across the visual field
- Rapid loss of peripheral (side) vision
- Sudden decrease in central vision clarity
- Fixed visual field defects
Persistent abnormal flashes:
- Frequent flashes persisting for hours or days
- Flashes are visible with eyes closed
- Flashes accompanied by multiple new floaters
Associated symptoms:
- Eye pain or unusual pressure sensation
- Severe headache with visual changes
- Light sensitivity (photophobia)
- Recent eye trauma with new visual symptoms
Remember: Retinal emergencies are typically painless, so the absence of discomfort doesn’t rule out serious conditions.
Serious Underlying Conditions
While most flashes and floaters result from benign vitreous changes, they can sometimes indicate sight-threatening conditions requiring urgent intervention.
Retinal Detachment
Retinal detachment occurs when the retina separates from its underlying support tissue, cutting off its blood supply. Without immediate treatment, this condition leads to permanent vision loss.
Key statistics:
- Annual incidence: 12.17 per 100,000 people globally
- Higher rates in myopic individuals: up to 868.83 per 100,000 in high myopes
- Peak occurrence: ages 50-70, though it can happen at any age
Warning signs include:
- Sudden onset of numerous floaters
- Repeated flashes of light
- Progressive “curtain” or shadow in peripheral vision
- Rapid loss of visual field
Treatment timeline: Studies consistently show that intervention within 24-48 hours significantly improves visual outcomes compared to delayed treatment.
Posterior Vitreous Detachment (PVD)
PVD represents the natural separation of vitreous gel from the retina—a normal aging process affecting about 75% of people over age 65. While usually benign, PVD can occasionally cause complications.
Typical PVD progression:
- Initial symptoms: Large floater (often described as “cobweb”) with flashes
- Duration: Symptoms gradually improve over 3-6 months
- Risk period: The First 6 weeks carry the highest risk for retinal tears
- Bilateral occurrence: The Second eye is often affected within one year
Research findings: A 2024 study of 1,010 patients found that 9.9% of those with confirmed PVD developed retinal tears, emphasizing the importance of prompt professional evaluation.
Retinal Tears
Sometimes during PVD, the vitreous can tear the retina if adhesions are particularly strong. Retinal tears require immediate treatment to prevent progression to detachment.
High-risk locations:
- Areas of lattice degeneration
- Sites of previous eye trauma
- Regions of abnormal vitreoretinal adhesion
- The peripheral retina, where vitreous attachments are strongest
Other Serious Conditions
Vitreous hemorrhage: Bleeding into the vitreous cavity, often from:
- Diabetic retinopathy complications
- Retinal vein occlusions
- Trauma-related vessel rupture
- Age-related macular degeneration
Uveitis: Inflammatory conditions causing floaters alongside:
- Eye redness and pain
- Light sensitivity
- Blurred vision
- Potential systemic disease associations
Diabetic retinopathy: Advanced diabetes complications leading to:
- Retinal blood vessel damage
- Vitreous bleeding
- Progressive vision loss if untreated
Risk Factors by Age Group
Understanding your age-specific risks for flashes and floaters helps inform when symptoms warrant immediate versus routine evaluation.
Ages 20-40: Early-Onset Considerations
Floater prevalence: Less common but can occur, particularly with:
- High myopia: Nearsightedness >6 diopters significantly increases risk
- Eye trauma: Previous injuries disrupting the vitreous structure
- Inflammatory conditions: Uveitis or other ocular inflammation
- Genetic factors: Family history of early vitreous changes
Key insight: Recent research shows that 71.4% of healthy individuals under age 20 already show early PVD changes on advanced imaging, suggesting the process begins much earlier than previously thought.
Ages 40-50: Transitional Period
Common experiences:
- First awareness of occasional floaters
- Gradual vitreous liquefaction begins
- Increased myopia-related risks become apparent
- Presbyopia development coincides with vitreous changes
Monitoring approach: Annual comprehensive eye exams become increasingly important for early detection of problematic changes.
Ages 50-65: Peak Symptom Development
Highest incidence period:
- PVD onset: Most people develop symptomatic vitreous changes
- Retinal tear risk: Peak age for vitreoretinal complications
- Gender differences: Women may experience faster PVD progression after age 60
Statistical modeling: Research suggests that at age 50, the average time to complete PVD is 9 years, decreasing to 8 years by age 60.
Ages 65+: Advanced Changes
Expected developments:
- 75% prevalence: About three-quarters of individuals experience PVD
- Bilateral involvement: The Second eye is typically affected within 1-2 years
- Stabilization: Most symptoms improve as vitreous changes stabilize
- Complication awareness: Continued vigilance needed for sudden changes
High-Risk Populations
Myopic individuals:
- 3.5x higher risk for moderate-to-severe floaters
- Earlier onset of vitreous degenerative changes
- Increased retinal detachment risk throughout life
Previous eye surgery patients:
- Cataract surgery can trigger PVD within weeks to months
- 1 in 500 cataract patients develop retinal detachment within one year
- Lattice degeneration increases post-surgical risks significantly
- Higher risk of vitreous hemorrhage
- Blood vessel fragility leads to bleeding complications
- Regular retinal monitoring is essential for early detection
When to Seek Professional Care
Knowing when flashes and floaters require immediate versus routine evaluation can be challenging. Here’s a practical framework for making these critical decisions:
Immediate Emergency Care (Same Day)
Call your eye doctor immediately or visit an emergency room if you experience:
High-priority symptoms:
- Sudden shower of dozens of new floaters
- Curtain, shadow, or “shade” blocking part of your vision
- Significant loss of peripheral vision
- Flashes persisting for hours with new floaters
- Any vision loss accompanying floaters or flashes
Post-trauma concerns:
- New visual symptoms after eye or head injury
- Even minor trauma with a subsequent floater increase
- Sports-related impacts on vision changes
Associated red flags:
- Severe eye pain with visual symptoms
- Sudden onset after vigorous physical activity
- Symptoms following eye injection or surgery
Urgent Care (Within 24-48 Hours)
Schedule prompt evaluation for:
Moderate concern symptoms:
- Several new floaters are appearing over 2-3 days
- Noticeable change in existing floater patterns
- Mild flashes without other symptoms
- First-time floaters in high-risk individuals
Monitoring situations:
- Recent PVD diagnosis requiring follow-up
- Known retinal degenerative changes
- Family history of retinal detachment with new symptoms
Routine Monitoring (Next Available Appointment)
Annual exam timing appropriate for:
Stable, long-standing symptoms:
- Floaters present for months/years without change
- Occasional mild flashes in elderly patients
- Previously evaluated symptoms with normal findings
Preventive care scenarios:
- High myopia requiring regular monitoring
- Diabetic eye surveillance programs
- Age-appropriate screening schedules
The Poudre Valley Eyecare Approach
Our Fort Collins practice follows evidence-based protocols for flashes and floaters evaluation:
Emergency assessment includes:
- Same-day dilated retinal examination
- Advanced OCT imaging when indicated
- Comprehensive peripheral retinal evaluation
- Immediate treatment coordination if needed
Follow-up protocols:
- Risk-stratified monitoring schedules
- Patient education on warning signs
- Coordination with retinal specialists when appropriate
Technology advantages:
- Modern imaging capabilities for early detection
- 25+ years of experience recognizing subtle warning signs
- Medicare and Medicaid acceptance ensure access to care
Latest Research and Treatment Advances
Understanding the science behind flashes and floaters helps patients make informed decisions about their eye health. Recent research has significantly advanced our knowledge of these common symptoms.
Current Understanding
Recent advances in eye imaging technology have revolutionized our ability to study vitreous changes and risk factors. Optical Coherence Tomography (OCT) now allows eye doctors to visualize vitreous structure changes that were previously undetectable.
2025 prevalence data reveal that floaters affect up to 76% of the general population, with 33% reporting noticeable visual impairment. The incidence is significantly higher in people with myopia (3.5x risk) and hyperopia (4.4x risk) compared to those with normal vision. Understanding these patterns helps doctors identify high-risk patients and provide appropriate monitoring strategies.
Treatment Advances
YAG Laser Vitreolysis: Modern laser treatment represents a significant advancement for patients with bothersome floaters. A comprehensive 2024 study demonstrated that specialized laser therapy achieved floater reduction in 93.7% of patients over 6 months. However, this treatment is suitable only for specific floater types and requires careful patient selection.
Treatment considerations:
- Best results with isolated, well-defined floaters
- Pseudophakic (post-cataract surgery) eyes are ideal candidates
- Multiple sessions may be required for optimal results
- Experienced practitioners are essential for safety
Improved Vitrectomy Techniques: Modern surgical approaches using smaller-gauge instruments have dramatically reduced complications while improving outcomes. Recent research involving 195 eyes demonstrated successful floater removal with a 94.1% reduction in vitreous opacity using advanced surgical protocols.
Safety improvements include:
- 23-gauge and 25-gauge microsurgical instruments
- Reduced incision size, minimizing trauma
- Advanced visualization systems for precision
- Lower complication rates compared to traditional techniques
Early Detection Benefits
Research consistently demonstrates that retinal tears detected within 24-48 hours have significantly better treatment outcomes than delayed cases. This finding underscores the importance of prompt evaluation when warning signs appear.
Diagnostic advances:
- Ultra-widefield retinal imaging captures peripheral pathology
- OCT angiography reveals subtle vascular changes
- Automated image analysis assists in early detection
- Telemedicine options expand access to specialist consultation
Emerging Therapies
Nanobubble technology: Scientists are developing innovative treatments using targeted nanobubbles to break apart floaters less invasively than current laser or surgical methods.
Pharmacologic approaches: Research into medications that could prevent or treat vitreous degenerative changes shows early promise, though clinical applications remain years away.
Artificial intelligence integration: Machine learning algorithms are being developed to analyze retinal images and predict which patients are at the highest risk for complications.
Living with Benign Symptoms
For patients with confirmed benign flashes and floaters, several strategies can help minimize their impact on daily life while maintaining optimal eye health.
Natural Adaptation Process
Most people find that bothersome floaters become less noticeable over time through a process called neuroadaptation. Your brain gradually learns to filter out consistent visual disturbances, similar to how you stop noticing background noise.
Adaptation timeline:
- Initial weeks: Symptoms are most bothersome and noticeable
- 1-3 months: Gradual decrease in symptom awareness
- 6+ months: Significant improvement in most patients
- Ongoing: Occasional awareness but minimal impact
Practical Management Tips
Eye movement techniques:
- Gently shift your gaze up and down to temporarily move floaters
- Avoid excessive eye rubbing, which can worsen symptoms
- Use normal blinking patterns to redistribute tear film
Environmental modifications:
- Adjust lighting to minimize floater visibility
- Use softer illumination when reading
- Consider polarized sunglasses for outdoor activities
- Position computer screens to reduce background glare
Lifestyle considerations:
- Stay well-hydrated to support vitreous health
- Maintain regular sleep schedules for optimal eye function
- Manage blood pressure and diabetes if applicable
- Continue normal activities without restriction
When Symptoms Persist
For the minority of patients whose floaters significantly impact daily function despite adaptation, treatment options may be considered:
Candidacy evaluation:
- Comprehensive symptom assessment
- Objective measurement of visual impact
- Discussion of risks versus benefits
- Second opinion consultation if appropriate
Treatment timing: Most specialists recommend waiting at least 6 months after symptom onset before considering intervention, allowing time for natural adaptation.
Prevention and Eye Health
While age-related vitreous changes cannot be prevented entirely, maintaining optimal eye health may help minimize complications and preserve vision throughout life.
Systemic Health Management
- Maintain HbA1c levels below 7% when possible
- Regular endocrinologist follow-up
- Annual dilated retinal examinations
- Prompt attention to any vision changes
Blood pressure management:
- Target levels appropriate for your age and health status
- Medication compliance as prescribed
- Regular monitoring and adjustment
- Lifestyle modifications supporting cardiovascular health
Nutrition for eye health:
- Omega-3 fatty acids from fish or supplements
- Antioxidant-rich foods (leafy greens, berries, citrus fruits)
- Adequate hydration supporting vitreous clarity
- Vitamin supplements as recommended by your doctor
Protective Measures
Eye safety practices:
- Safety glasses during sports or hazardous activities
- Proper eye protection in work environments
- Careful handling of chemicals or projectiles
- Immediate medical attention for any eye trauma
- Quality sunglasses with UV-A and UV-B protection
- Wide-brimmed hats during prolonged sun exposure
- Awareness of reflected UV from snow, water, or pavement
Regular monitoring:
- Age-appropriate comprehensive eye examinations
- Adherence to recommended follow-up schedules
- Prompt reporting of any vision changes
- Understanding your personal risk factors
Risk Factor Modification
- Proper corrective lens prescriptions
- Regular eye strain breaks during near work
- Outdoor time for children to slow myopia progression
- Specialized contact lenses or treatments when appropriate
Lifestyle factors:
- Regular exercise supports overall circulation
- Smoking cessation to reduce vascular damage
- Moderate alcohol consumption
- Stress management techniques
Additional Resources and Citations
For those seeking additional information about flashes and floaters, the following authoritative medical resources provide comprehensive, evidence-based information:
1. American Society of Retina Specialists – Posterior Vitreous Detachment
Source: https://www.asrs.org/patients/retinal-diseases/9/posterior-vitreous-detachment
The American Society of Retina Specialists provides detailed patient education about posterior vitreous detachment, the most common cause of new flashes and floaters. This resource explains the natural progression of PVD, risk factors including myopia and age, and when symptoms require immediate evaluation. The ASRS emphasizes that while 85% of PVD cases develop without complications, the first 6 weeks following symptom onset carry the highest risk for retinal tears or detachment.
2. Harvard Health Publishing – Floaters and Flashes in the Eye
Harvard Medical School’s comprehensive overview addresses key warning signs that require immediate medical attention, including the sudden onset of multiple floaters, persistent flashes, and vision changes. The resource emphasizes that while most flashes and floaters are harmless, sudden changes warrant prompt ophthalmologic evaluation to prevent potential vision loss from retinal complications.
3. National Center for Biotechnology Information – Floater Prevalence Study
Source: https://pmc.ncbi.nlm.nih.gov/articles/PMC3693028/
This peer-reviewed research study of 603 smartphone users found that 76% of participants experience floaters, with 33% reporting noticeable visual impairment. The study identified increased risk in myopic and hyperopic individuals and provides current epidemiological data supporting the high prevalence of flashes and floaters in the general population, particularly among technology users and younger demographics.
Conclusion
Understanding the difference between normal flashes and floaters versus emergency warning signs could literally save your sight. While most flashes and floaters are harmless parts of aging, the serious conditions they sometimes indicate require immediate treatment to prevent permanent vision loss.
Remember these critical warning signs demanding immediate professional attention:
- Sudden shower of new floaters
- Curtain or shadow in your vision
- Persistent flashes with other symptoms
- Any significant vision changes accompanying floaters or flashes
Don’t wait if you’re experiencing new or worsening flashes and floaters—early intervention often makes the difference between preserving your vision and facing permanent loss. Contact our Fort Collins practice today to schedule an evaluation with our experienced team.
Your sight is irreplaceable. Trust it to Northern Colorado’s most experienced eye care professionals.
FAQs
-
Floaters are small dark dots, squiggly lines, or cobweb-like shapes drifting in your vision. Flashes appear as brief lightning-like streaks of light, often at the edge of vision, caused by vitreous gel tugging on the retina.
Please note: None of the above should be considered medical advice. If you’re having any concerns about your vision, please reach out to us immediately or see your primary care provider.